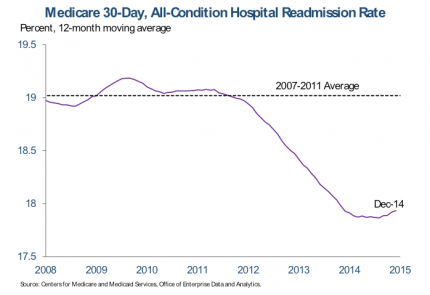
Improving population health begins with focusing on the health of each one of your patients. To do so, we in the healthcare community—nurses and physicians alike, need to identify and engage patients—particularly those of high risk—throughout the continuum of care. These are individuals most likely to be readmitted, miss an appointment, skip medications or unable to pay their bill.
But how can we pinpoint these individuals efficiently when we’re often looking at multiple databases and EHRs, examining enormous quantities of unstructured data—from multiple notes fields and categories, pathology reports, radiology notes, to admission notes and everything in between—containing invaluable historical information, all entered at different times, in different ways by different people?
Standard EHR systems do not currently provide a way to easily synthesize and summarize patient information on the changing risk factors recorded in different EHRs to support clinical decision-making. In addition, EHRs do not capture all the data points to understand the risks patients face, nor does it prioritize care for those at high risk for readmissions or infections. Imagine then how much we could do to identify, treat and engage patients if we had a way to analyze unstructured data!
The primary benefit of normalizing and aggregating unstructured data is attaining a cohesive picture of the patient’s history, diagnosis, treatment, and outcome. If details around the pathology of a patient’s tumor are only recorded within the pathology note for example, then analysis cannot include such things as genomics, margin reports, laterality, size, shape or even perhaps the stage of the tumor. Including that information along with trends for an individual patient or an entire population could be valuable. Additionally, combining that information with data about the treatment and outcome of a patient—which is possibly available within textual notes fields—can provide a rich field for research and results-driven treatment.
Here at CareSkore, we thrive to compile—and where applicable—translate data from hospitals electronically. Through our Personalized Population Management™ platform, we’re able to identify patients at high risk of readmission and hospitalization by combining clinical and 3rd party data. We put in place standard care plans so everyone on the team knows the steps they should be taking to manage the patients. CareSkore also allows our partners to reach out to patients even after they have left the nursing facility, using our Iris module, and document the follow-up care to provide them resources as needed.
Fundamentally, integrated care management, leveraged by data and predictive analytics, helps nursing home administrators to:
- Identify and engage patient populations at-risk for poor outcomes or unnecessary intervention at a time of need and opportunity for impact
- Perform assessments and respond to changes in patients’ conditions to uncover problems that, if addressed through effective interventions, will improve care and reduce the need for expensive services—particularly ER visits and hospitalizations
- Collaborate with patients and their caregivers as well as primary care, specialty, behavioral health, and social service providers and show hospital partners they can perform proper follow-up care
- Have an integrated system that provides a complete picture of expenditures and combines risk prediction software, chronic disease criteria, or utilization thresholds with patient-to-provider referrals or assessments
- Combines the strengths of both quantitative and qualitative approaches and brings data together from multiple sources
All in all, benefits extend beyond medical issues to address, to the extent possible, how patients’ psychosocial circumstances affect their ability to follow treatment recommendations and achieve a healthy lifestyle. The goals are to maintain or improve patients’ functional status, increase their capacity to self-manage their condition, eliminate unnecessary clinical testing, and reduce the need for acute care services.
The result? Fewer nursing visits, shorter hospital stays, better intra-office communication, faster and efficient communication between primary physician and nursing facilities, and cost savings that could pay for the expansion of EMR use in those facilities.
This post is an edited version originally published on McKnights.