While there are many definitions of population health or the “health outcomes of a group of people”, the terms place emphasis on the determinants of health and the interventions to elevate overall health status. Population health is often used interchangeably with public health to describe the activities conducted by governmental public health agencies, community and national organizations to improve the health of a community.
Promoting health and preventing disease are key components of population health, both at the societal level and within a primary care practice. And within that, there are three different levels of prevention:
1. Primary prevention – Prevention strategies that seek to prevent disease or injury, generally through reducing exposure or risk factor levels. These strategies can reduce or eliminate risk factors (risk reduction).
2. Secondary prevention – Prevention strategies that identify and control disease
processes in their early stages before signs and symptoms develop (screening and treatment).
3. Tertiary prevention – Prevention strategies that prevent disability by restoring individuals to their optimal level of functioning after a disease or injury is established and damage is done.
The goals of population health are to help physicians engage in preventive care, improve care quality, and ultimately, improve health outcomes. There are several benefits of applying a population focus to primary care. Population health tools—especially ones that leverage analytics—allow providers to track care across all of their patients, rather than limiting their attention to the patients who make appointments. One provider explained that “I thought I was doing a really good job” by discussing preventive care during annual physicals or acute visits. However, since adopting a more systematic method of monitoring all of her patients, she said, “now it seems that was not the case. We could not pull all the charts to see who needed [a preventive visit].”
Based on the 2017 healthcare reform landscape, there are six areas of initiatives that are currently shaping population health:
Wellness / Preventive health
The second most widely adopted initiative promotes workplace health, school health, weight loss and smoking cessation and are typically implemented to improve overall health and deter more serious conditions from occurring. This initiative category dropped from 79 percent in 2015 to 72 percent in 2016.
Clinically Integrated Network (CIN)
Another model of care, CIN, is a health network of providers/hospitals that use protocols to improve care, lower costs and increase value to a particular market. Roughly half of study organizations with initiatives in place in 2016 leverage this model of care for population health.
Patient-Centered Medical Home (PCMH)
Focuses on acute, chronic and preventative care that is coordinated and integrated across multiple sites with health quality and safety in mind. Care across the continuum could be proving to be difficult as approximately 50 percent of study organizations indicated they utilize this model of care in 2015 and 2016.
At-risk payment structures
At-risk payment structures include Accountable Care, Medicare Shared Savings Program, bundled payment, and employer contracts. An increase in this category since last year indicates the organizational shift to value-based payment but significant gains could take some time as organizations build out their population health programs.
At-risk cost structure
The least adopted program includes Medicare Advantage plans, Medicaid managed care, commercial plan, and self-insured employee plans. This particular initiative grew from roughly 17 percent in 2015 to 19 percent in 2016.
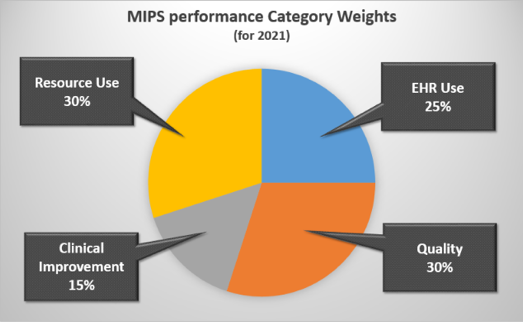
MACRA will certainly impact population health in 2017. MACRA was enacted in 2015 to replace the Sustainable Growth Rate (SGR) for physician payment. In 2016, new rules were issued for quality reporting and payment policies that will substantially change the status quo for Medicare’s physician reimbursement in 2017.
Get more in-depth information on the MACRA Quality Payment Program and learn more about Physician Focused Payment Models (PFPMs) Technical Committee.
As a physician, below are a few tips to get ready for the new MACRA:
- Attend webinars.
- Request a CMS speaker to give your group more details about the Quality Payment Program.
Although hospitals have been subject to the performance-based payment provisions of the Affordable Care Act (ACA), the concept is new to physicians, who need to understand how to improve performance and avoid payment penalties. In essence, this will entail developing more complex governance models, adjusting to more data sharing across the care continuum, and more performance measurement.
With a choice of payment models, physicians will need to conduct financial planning to determine which path presents the greatest benefit given current performance.
Once a payment model is selected, physicians must decide how to organize. Understanding that unprecedented levels of partner collaboration, testing, and co-innovation will be the keys to long-term success.